Background
The newly published molecular International Prognostic Scoring System (IPSS-M) represents a powerful risk stratification tool for treatment decision-making in myelodysplastic neoplasms (MDS); however, its utility in the context of allogeneic hematopoietic stem cell transplantation (allo-HSCT) remains to be fully explored.
Methods
We retrospectively analyzed a large multicenter cohort of 347 MDS patients who underwent allo-HSCT between January 2017 and October 2022. The prediction accuracy of IPSS-M at diagnosis for 3-year survival outcomes was assessed and compared to that of the conventional revised International Prognostic Scoring System (IPSS-R).
Results
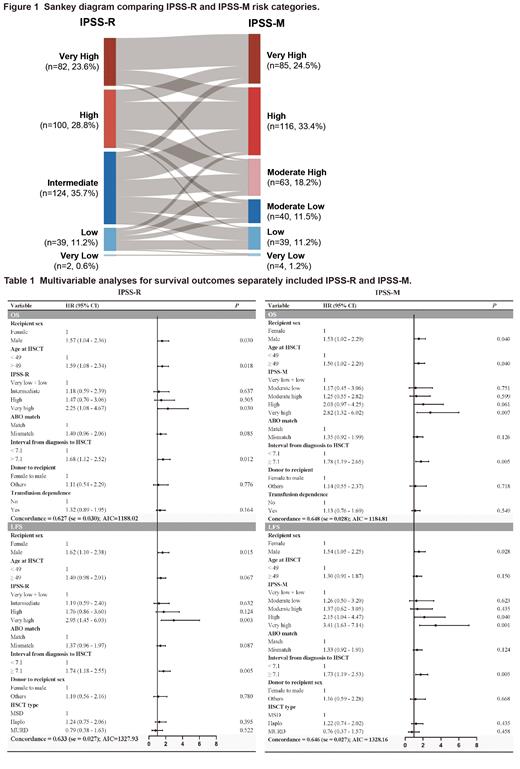
Among the 347 patients, median age at transplant was 48.3 years and 41.2% of patients were female. According to IPSS-M, patients were clustered as very low risk (1.2%), low risk (11.2%), moderately low risk (11.5%), moderately high risk (18.2%), high risk (33.4%), and very high risk (24.5%), resulting in a restratification of 49.3% of the entire cohort when compared with IPSS-R. Of these reclassified patients, 52.6% patients were upstaged and 47.4% were downstaged. Median follow-up time among the survivors was 28.6 (range, 4.7 to 76.6) months. With the IPSS-M model, overall survival (OS) and leukemia-free survival (LFS) discrimination was refined relative to the IPSS-R as evidenced by a 7.0 percentage- and 5.7 percentage-point increase in the concordance index (C-index), which was further supported by the lower Akaike Information Criterion and higher C-indexes in multivariate analyses. Among patients undergoing haploidentical HSCT, IPSS-M model also demonstrated significantly improved prognostic performance for LFS versus IPSS-R (C-index, 0.707 vs 0.604) which was validated by multivariate analyses. When restricting our analyses to younger patients (<49 years) and patients carrying detectable mutations, IPSS-M retained greater prognostic value with respect to OS and LFS; while it failed to stratify individual probability of OS and LFS in their counterparts.
Conclusions
IPSS-M was confirmed to increase prognostic discrimination at the individual level and is applicable to transplant-specific settings, which also had an advantage for subjects carrying mutations and younger patients.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal